By the age of 50, 1 out of 4 men will have some cancerous cells in his prostate. At age 80, the ratio becomes 1 in 2. However, most men outlive their diagnosis.
WHAT ARE THE SYMPTOMS?
Prostate cancer develops slowly and does not typically cause symptoms at an early “stage,” when it is confined to the prostate. Symptoms may be related to the growth of cancer within or outside of the prostate and may include:
- Difficulty or an inability to urinate;
- Blood in urine;
- Painful ejaculation;
- Loss of appetite and weight; and/or
- Continual lower back, pelvic, or upper thigh pain.
Many of these symptoms can be caused by benign (non-cancerous) conditions and should be evaluated by a healthcare professional.
CAUSES AND RISK FACTORS
It isn’t entirely known what causes prostate cancer. Most prostate cancers are related to aging. Some prostate cancers may be inherited and caused by genetic mutations.
Risk factors include:
- Age: The older a man is, the higher his risk of prostate cancer.
- Race: African-American men have higher risk than American men of other ethnicities. Asian-American men have the lowest rates.
- Family history: Rates may increase if a person’s father or brother has the disease. Also, additional cancers in the family (particularly breast, pancreatic, ovarian) may increase risk.
- Diet: Some researchers have linked a high-fat diet to prostate cancer. Diets rich in lycopene (e.g. in tomatoes) or soy products may provide lower risk.
DIAGNOSIS
Prostate cancer is diagnosed through a biopsy, or the removal of small amounts of of prostate tissue with a needle. However, biopsies are not performed on all men. Biopsy may be indicated if a man has:
- A persistently elevated PSA (“prostate specific antigen”) blood test;
- A rising PSA; and/or
- An abnormal digital rectal examination (described below).
PSA is a chemical made by the prostate that is associated with prostate cancer risk; higher levels mean higher risk.
There are different recommendations for when to start “screening” for prostate cancer. The American Cancer Society recommends having a discussion about the risks and benefits of screening in men starting at age 50. Men with additional risk factors (e.g. African American descent, family history) should have these discussions earlier (ages 40-45). Men should not have screening if they have less than 10 years life expectancy.
An elevated PSA level does not always indicate cancer. Prostate enlargement, inflammation, and other factors can increase the PSA level. Therefore, to determine the need for a biopsy, providers may also order or evaluate the following:
- Free PSA: This test measures the percentage of free PSA (PSA that is not bound to other molecules) in the blood. A low percentage of free PSA indicates a greater risk of having prostate cancer.
- PSA velocity: PSA velocity is the annual rate at which the PSA increases. This rate can be associated with higher risk of cancer.
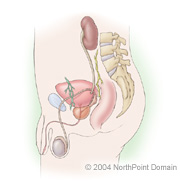
- Digital rectal exam: In this test, the provider inserts a finger in the rectum to feel the prostate gland. Abnormally firm areas may be associated with cancer.
- PSA density: Providers divide the PSA number by the prostate volume (size) to assess the likelihood of cancer; this takes into account the fact that prostate enlargement, which is common in men as they age, can lead to a higher PSA level. An elevated PSA density suggests increased risk.
- Novel biomarkers: There are newer blood and urine tests that can check a man’s risk of prostate cancer more accurately, when the PSA may only be slightly elevated or the level of risk is unclear. Some of these tests including the 4K score, Prostate Health Index, ExosomeDx, and Select MDx.
- Imaging: Prostate MRI (also called “multiparametric MRI”) is a common imaging test to evaluate risk of prostate cancer. MRI provides a score to give the likelihood that one will find cancer on a biopsy. Also, MRI can provide a “target” that can be used during a biopsy to improve its accuracy.
Certain imaging (radiology) tests help assess the extent of the prostate.
- Magnetic resonance imaging (MRI): This is the most common test to evaluate whether cancer has grown beyond the prostate within the pelvis.
- PSMA PET scan: This is the best test to evaluate for spread of prostate cancer in the body (e.g. to lymph nodes, bone).
- Bone scan: This is used less commonly due to the availability of more accurate staging tests (e.g. PSMA PET)
- Computed tomography (CT) scans: As above, this is used less commonly due to the availability of more accurate tests.
TREATMENT APPROACH
Treatment for men with prostate cancer depends on:
- The man’s age and life expectancy;
- His feelings about the side effects associated with each treatment;
- The grade (“Gleason score”) and stage (extent) of the cancer; and
- Other health conditions.
The active treatments for prostate cancer include:
- Surgery, or removing cancer, typically with a robotic surgical system (the “daVinci” robot); this is a minimally invasive approach to surgery that speeds up recovery and minimizes risk of bleeding.
- Radiation, or using high-dose external x-ray beams or radioactive seeds to kill cancer cells; these can be done with different approaches (e.g. IMRT, SBRT), in different combinations (e.g. external beam + brachytherapy boost), and potentially in combination with medication (e.g. hormone therapy.
- Ablation, or destruction of cancer cells with probes within the prostate treating, typically treating just a portion of the prostate (“focal therapy”) (e.g. irreversible electroporation [Nanoknife], HIFU, cryotherapy);
- Hormone therapy, which can slow or stop cancer growth by decreasing the testosterone level; and
- Chemotherapy, or using drugs to kill cancer cells; this is reserved for prostate cancer that has spread to multiple parts of the body
Monitoring rather than treatment of prostate cancer is very common, as many prostate cancers that are diagnosed are slow-growing. This approach allows for patients to avoid the side effects and risks of treatment while monitoring for signs of progression, and changing to a treatment approach should this occur:
- Active surveillance: this is a more active approach to monitoring prostate cancer, with a schedule of checking PSA, repeating imaging (MRI), and repeating biopsies at certain intervals. Other tests can be used to assess risk of progression (e.g. genomic tests).
- Watchful waiting: this is a more passive approach to monitoring typically in older men with other significant health problems, in which men are monitored based on their symptoms to determine whether treatment is necessary.
Our team at Brown Urology is part of a fully integrated, multidisciplinary team to diagnose and treat prostate cancer at any level, while providing individualized counseling to ensure patients’ preferences are met regarding how they want to proceed through diagnostic and treatment pathways.
We work closely in an interdisciplinary team with radiation oncology, medical oncology, social work, genetics, nutrition, and others to ensure patients have a holistic approach to their care.
Our team members collaborate with providers at the Lifespan Cancer Institute to leverage all of the resources of our institution to help patients. We have multiple open clinical trials to offer men access to novel approaches to treatment of localized and advanced prostate cancer.
Further, we have a robust program in survivorship to help men recover from treatments from prostate cancer, particularly in terms of urinary and sexual function. Our patients work with pelvic floor physical therapists to optimize urinary control after treatment, as well as the men’s health clinic to discuss and plan for “penile rehabilitation”, or recovery of erectile function after treatment.
This material cannot be reproduced in digital or printed form without the express consent of NorthPoint Domain, Inc. Unauthorized copying or distribution of NorthPoint Domain’s Content is an infringement of the copyright holder’s rights.